Professor Kwang-Soo Kim, the director of the Molecular Neurobiology Laboratory at McLean Hospital, and the McLean-Massachusetts General Hospital team have provided the world’s first successful case of treating a patient with Parkinson’s disease (PD) by reprogramming the patient’s own skin cells into dopamine neurons and implanting it into their brain. Professor Kim received his PhD and MS degrees from KAIST and is also a professor of psychiatry at the Harvard Medical School.
Parkinson’s disease is one of the most common degenerative nervous system diseases, along with dementia and stroke. The disease occurs due to the death of the nerve cells that secrete the dopamine neurotransmitter, causing symptoms such as muscle tremors, slow movement, stiffness of the body, and walking and speech disorders.
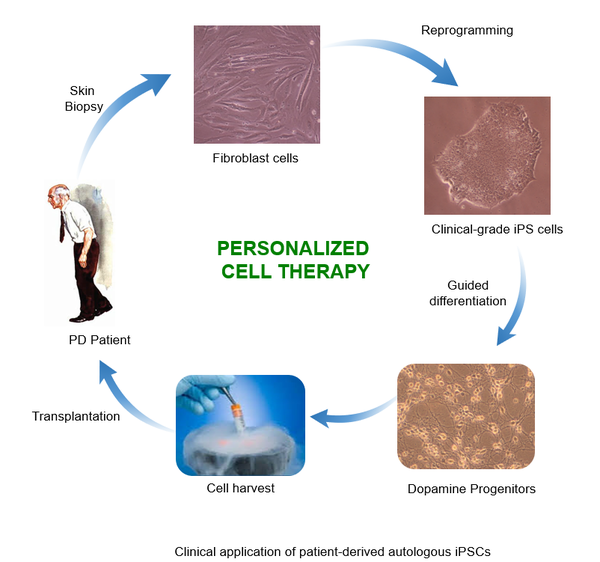
The treatment used the induced pluripotent stem cells (iPS) technology, pioneered by the 2012 Nobel Prize in Physiology or Medicine winner Shinya Yamanaka. This is the world’s first successful treatment using the patient’s own iPS cells. By reprogramming and transplanting the patient’s own skin cells, the risk of rejection by the body’s immune system is greatly reduced, and the indefinite propagation of these cells means exceptional regenerative capabilities.
Due to the demand for a highly efficient method for a PD treatment without any side effects, the research team has been focused on treatment technologies for a long period. In 2009 and 2011, they reported the development of a technique to produce iPS cells without the use of viruses and showed the possibility of applying it to an animal model. They have also reported an efficient mechanism for stem cell differentiation (the transformation of a cell into a different type) by investigating the differentiation mechanism of dopamine cells. In 2017, they developed a dedifferentiation technology (the regression of a specialized cell into a simpler one, like a stem cell) that can be clinically applied. In 2020, they used an animal model and their previous technologies to show improvement of PD symptoms without side effects such as cancer.
Through the approval and request of the FDA, a 69-year-old Parkinson’s patient, George Lopez, was treated over two clinical trials in 2017 and 2018. The transplanted dopamine neurons showed no signs of immune system rejection. After continuous testing for two years post-surgery, the stable improvement of the patient had the team deem the treatment successful in May.
Dr. Jeffrey Schweitzer of the Massachusetts General Hospital, who conducted the transplant surgery on Lopez, stated that while only from a single patient, these results were “extremely encouraging”. Professor Kwang noted that more clinical trials are required to prove the stability and efficiency of this new treatment. He plans to continue with follow-up research for about 10 more years and hopes that personalized cell therapy will become a universal treatment for PD in the future.

