As the COVID-19 pandemic continues, the ability to predict pathways of infection and to identify those most at risk is very important. To this end, a research group from the Graduate School of Medical Science and Engineering has pinpointed a method to identify patients who are more likely to experience severe symptoms of the coronavirus. Published in Frontiers in Immunology on August 28, their paper describes a biomarker that correlates with more serious COVID-19 cases.
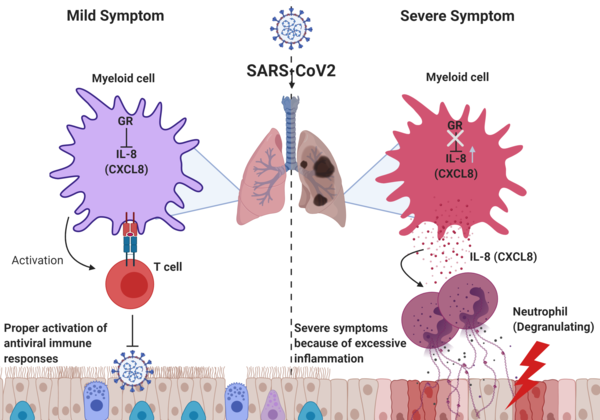
When infected with SARS-CoV-2, people’s immune systems may respond differently, resulting in a range of symptoms. Using publicly available data from the Shenzhen Third People’s Hospital in China, Professor Heung Kyu Lee and PhD candidate Jang Hyun Park analyzed the differences between airway cells of patients who had minimal symptoms and those with more severe outcomes. The analysis revealed a negative association between the level of neutrophils, a type of white blood cell in the immune system, and the amount of cell receptors for glucocorticoid, a steroid hormone that can be used as an anti-inflammatory drug to treat COVID-19 symptoms. This means that patients with high levels of neutrophils are more likely to become seriously ill, and are less able to respond to treatment due to the lack of glucocorticoid cell receptors.
Although neutrophils are a natural and necessary part of a healthy immune system, when there are too many — and not enough of other types of white blood cells — they can cause inflammation that damages the airway and lungs. Acute respiratory distress syndrome (ARDS), which is a result of this inflammation, has been responsible for around 70% of confirmed COVID-19 deaths. Therefore, testing neutrophil count in patients before symptoms become serious will allow for better preparation and suitable treatment to be prescribed. Professor Lee commented that the “finding could be used as a biomarker for predicting disease severity in patients and thus selecting a targeted therapy that can help treat them at an appropriate time.”

